Stories

Michael Jankowski: Follow Your Passions and See Where They Lead
How do pain mechanisms produce our sense of pain, and how do they differ in children, teenagers, and adults? In his lab in the Department of Anesthesia at the Cincinnati Children’s Hospital Medical Center, Professor Michael Jankowski investigates the pain mechanisms at work over the course of our lives.
“We’re trying to understand the basic biology of these different systems across the lifespan,” said Jankowski, “so that we can develop targeted age-specific strategies for pain in different age populations.”
Jankowski didn’t set out to study pain initially, as he had plans to go to medical school and become a physician. As an undergraduate student at the University of Pittsburgh aiming to round out his medical school application, he worked in the lab of Susan Sesack studying basic neuroanatomy, and found himself captivated by the research.
“I really fell in love with it,” he said. “I quickly realized that research was a lot better fit for me than medicine.”
The Sesack group studied how different monoaminergic projections—or neurons that produce neurotransmitters like serotonin—regulate different brain regions and different brain circuits. Under Dr. Sesack’s mentorship, Jankowski learned neuroanatomy and studied neural circuity in the brain. His specific project focused on how brain stem serotonin neurons regulate the prefrontal cortex— the front part of the brain that is responsible for higher order thinking—specifically for circuits associated with depression. His work then expanded into tracing inhibitory pathways in the brain that parallel monoaminergic circuits. Jankowski continued in the Sesack lab to complete his master’s research.
After the influential time he spent with Dr. Sesack, Jankowski decided it was time to broaden his foundations as a researcher, combining developmental biology with molecular strategies. He joined Kathryn Albers’ lab for his Ph.D. research on developmental neuroscience. “I started investigating basic mechanisms of nerve regeneration and the role that transcription factors, regulatory proteins within sensory neurons, play in peripheral nerve regeneration,” he said.
After postdoctoral work with H. Richard Koerber, in 2011, Jankowski started his own lab at Cincinnati Children’s Hospital. He explains, “I had a background in anatomy, I had a background in nerve regeneration and molecular biology, I had experience in developmental neuroscience, and then sensory physiology. It made a lot of sense to then establish my lab in a way that looked at all of these things collectively, as well as adding on other factors such as behavioral analyses. That’s how I ended up in doing muscle pain work.”
In 2012, Jankowski received the Rita Allen Foundation Award in Pain.“ I knew some people who had received the Award in Pain; I knew Ted Price [RAF 2009] and Steve Prescott [RAF 2009]. I had some ideas about what I wanted to try. I threw the application out there and then within six months, I’m a Rita Allen Scholar. It was one of those things that happened very suddenly. But the impact it’s had has been enormous.”
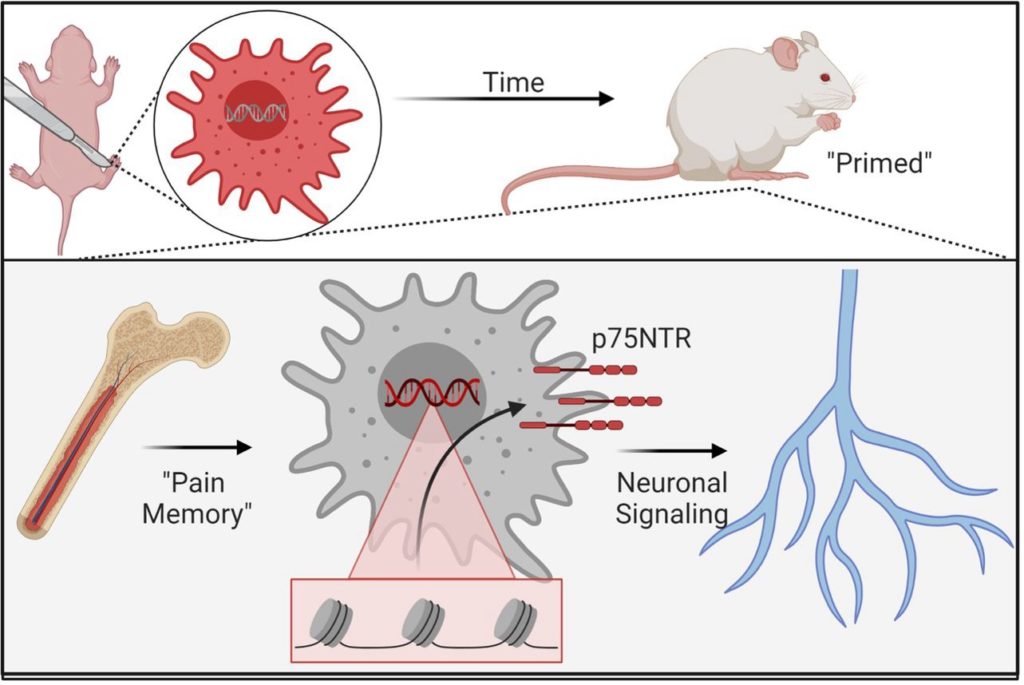
“After years of studying how nociceptors transduce information from the external environment to the central nervous system, we started looking at the multifunctional role of nociceptors. The first foray into this was looking at how pain fibers, or nociceptors, regulate cardiovascular reflexes. And then we started looking at how they regulated a lot of other things. Right now, we’re looking at how nociceptors modulate immune function in multiple tissues.
“What’s really intriguing about these fibers is that they communicate with immune cells to a very high degree. They produce cytokines and chemokines that regulate immune cell function in the target tissues. They’re not just afferents, as we like to call them, that signal from the outside to the inside. They’re also talking in the other direction, regulating immune function, regulating cardiovascular function, and speaking with the glial cells—non-neuronal cells that provides physical and chemical support to neurons and help maintain their environment—to control their functions. There are many multifunctional roles for sensory neurons,”
Over the years, Jankowski has seen the pain research field evolve and transform to include more interdisciplinary research. Pain researchers now understand how pain is connected to many different systems in the body like the immune system and the cardiovascular system. In addition, model systems are expanding to include human samples such as induced pluripotent stem cells and patient tissues.
“The Rita Allen Award is helping us understand how these sensory fibers that regulate pain do so many more things. And I think that’s the impact that we can have on the field moving forward.”
Jankowski has also worked on several collaborative projects with other Award in Pain Scholars—including Reza Shariff-Naeini (RAF 2013) and Becky Seal (RAF 2013)—and interdisciplinary projects with other Rita Allen Scholars who are not Pain Scholars. “With Sreekanth Chalasani (RAF 2012), for example, we got a grant together because he did some interesting work in channel biology, and I was interested in using it in neuroscience. I was able to make that collaboration because I knew him from the Rita Allen meetings. The types of connections and networking that the Rita Allen Foundation has created for us Scholars is unparalleled.”
Here, Jankowski shares the influence of the Award on his career trajectory, his biggest challenges, and advice to future applicants.
How did the award influence your research and career trajectory?
It opened the door to people wanting to do work with you. Your name recognition increases when you’re a Rita Allen Scholar, and that was so incredibly helpful to me. I don’t think I would ever be where I am right now without this award. It set me up on a trajectory going one way that I probably wouldn’t have had if I didn’t have this support.
I went from assistant professor to division director and now Vice Chief for Research in 13 years—that’s pretty fast. I was able to say in my application materials for other grants that I was externally funded within six months of starting my lab. Right after that, I got my first R01 and then I haven’t looked back since.
What are some of the biggest challenges you have had in your research?
Realizing that things are not always going to work and your hypothesis is probably wrong, but that’s okay. You want your hypothesis to be wrong. One thing that I always tell my trainees is that you want to be proven wrong because that’s how you actually test a hypothesis. You don’t test a hypothesis by proving your preconceived assumptions about something. It’s sort of counter intuitive, but that’s actually true.
What advice would you give to others who are looking to apply for the Award in Pain?
Given that it’s a three-year award, the advice I would give is make sure that your research is feasible. But also make it so that the project can further your research program as an independent investigator. This is not an R01-like proposal but there needs to be an understanding about how the support from the Award in Pain will facilitate your future research program. Having those little tidbits in there really helps.