Stories

Announcing the 2020 Rita Allen Foundation Award in Pain Scholars
Four pioneering early-career scientists will receive support to uncover the biology of pain.
The Rita Allen Foundation has named the 2020 class of Award in Pain Scholars, celebrating four early-career leaders in the biomedical sciences whose research holds exceptional promise for revealing new pathways to understand and treat chronic pain.
The selected Scholars will receive grants of $50,000 annually for up to three years to conduct innovative research on critical topics on the biological mechanisms of pain—including how the nervous system distinguishes between soft and harsh stimuli, what role the immune system plays in chronic pain, and what makes individuals at risk for chronic pain after a traumatic injury.
Two awards are supported by the Rita Allen Foundation and two are supported by Open Philanthropy.
“By laying the foundations of biological knowledge, basic research holds the power to unlock new treatments, and improve our ability to safely reduce and treat chronic pain with far-reaching potential for individual and societal impact,” said Elizabeth Good Christopherson, President and Chief Executive Officer of the Rita Allen Foundation. “Together with Open Philanthropy, we are eager to follow the work of these emerging leaders in pain research as they advance a field rich with biological complexity and significance.”
Since 1976, the Rita Allen Foundation has awarded millions of dollars in grants to early-career biomedical scholars. These grants allow them to establish labs and pursue research directions with above-average risk and promise, including in the field of basic research on mechanisms that initiate and propagate pain signaling in the nervous system. Rita Allen Foundation Scholars have gone on to make transformative contributions to their fields of study, and have won recognition including the Nobel Prize in Physiology or Medicine, the National Medal of Science, the Wolf Prize in Medicine, and the Breakthrough Prize in Life Sciences.
Designed to recognize emerging scientists whose work holds high potential for uncovering new pathways to improve the treatment of chronic pain, since 2009 the Award in Pain has invested in 29 pain researchers at the early stages of their careers, enabling them to expand understanding of a complex neurobiological system with widespread societal impact.
The 2020 Award in Pain Scholars were selected by a committee that includes past Award in Pain recipients, as well as other leading pain researchers.
The members of the 2020 class of Rita Allen Foundation Award in Pain Scholars are:
Ishmail Abdus-Saboor, University of Pennsylvania
Geoffroy Laumet, Michigan State University
Sarah Linnstaedt, The University of North Carolina at Chapel Hill
Andrew J. Shepherd, The University of Texas, MD Anderson Cancer Center

Photo: Ed Newton for Burroughs Wellcome Fund
Ishmail Abdus-Saboor, University of Pennsylvania
Mitchell J. and Margo K. Blutt Presidential Assistant Professor, Biology
B.S., North Carolina A&T University
Ph.D., University of Pennsylvania
In conjunction with Open Philanthropy
My research focuses on a long-standing question—how does the nervous system encode a soft gentle caress versus a harsh painful stimulation? To accomplish this, I use neurobiology, computational biology, and mathematics to objectively measure pain—a sensory experience that is inherently subjective. Traditionally, researchers have applied sensory stimuli to the rodent paw and tried to infer the animal’s pain state based on the singular readout of whether the animal moved its paw or not. The problem is, animals will lift their paw to both innocuous and noxious stimuli; and with that sole measurement parameter, there is a high likelihood of incorrectly assigning the animal’s sensory experience. An innovation in our work is to use videography to take thousands of images per second to measure sub-second pain behaviors, and couple this with statistical modeling and machine learning to develop rodent “pain scales.”
What will funding from the Award in Pain allow you to do?
Individual susceptibility to pain is driven in large part by genetic variation. An interesting discovery my lab made while developing an automated pain scale is the identification of inbred mouse lines with unusual responsiveness to pain. Specifically, we identified mouse strains that responded to pain counter-intuitively; one mouse strain responded to painful touch like a soft stimulus, while another strain responded to soft touch like a deeply painful stimulus. These inbred mouse lines, which fail to respond normally to pain, may hold the keys to uncovering how populations of people have pathological pain sensitivity. This is significant because individuals with hypersensitivity to pain appear to have an increased risk of developing chronic pain. The Award in Pain will allow us to continue mapping behavioral responses at millisecond resolution in these outlier mouse strains across chronic pain states, with the goal of moving toward mechanistic detail.
How did you enter this career path? Was there anyone or anything that particularly inspired you?
I have been enamored with science since I was very young, and I knew that I wanted to be a scientist as early as third grade—despite never knowing any scientists personally. This early inclination to science was solidified in ninth grade when I set up a lab at home to investigate the regeneration rates of crayfish appendages when their drinking water was spiked with the herbal supplement ginseng. My parents had no qualms about a 14-year-old taking over an entire floor of the house with crayfish cages. They were, and continue to be, important sources of strength and encouragement for me. I won a first-place award in a citywide science fair for this project and since those high school days, a life in science is all I have ever desired.
What is your favorite science-related book?
As a postdoctoral fellow, I read the book The Challenge of Pain by Patrick D. Wall, which was published in 1982. In this book, Wall outlined his famous gate control theory of pain, which he developed alongside his colleague Ronald Melzack. While still theoretical at the time without experimental validation, the gate control theory of pain accounted for anecdotal and clinical findings related to spinal cord gating of pain, before messages reached the brain. Additionally, in the book, Wall described many case studies and clinical observations of pain that still baffle researchers to this day. As a scientist always looking for a challenge, reading Wall’s book convinced me that the pain field still has lots of mysteries to be uncovered and, just maybe, I could help solve a few of them.

Photo: Geoffroy Laumet
Geoffroy Laumet, Michigan State University
Assistant Professor, Physiology
Ph.D., Lille University School of Medicine, France
Our lab is interested in understanding why pain becomes chronic and how can we stop it. While it is obvious that neurons convey pain signaling throughout the body, neurons do not work in isolation and are constantly communicating with and getting influenced by other cells. We are particularly interested in the contribution of non-neuronal cells to chronic pain. We think that impaired communication between “pain-sensing” neurons and their surrounding cells may result in chronic pain. For example, we have discovered that anti-inflammatory molecules secreted by cells from the immune system prevent pain-sensing neurons from becoming persistently activated—this constant activity is the cellular basis of chronic pain. We hope that a better understanding of neuron/non-neuronal cell communication will lead to the development of new and better analgesics.
What will funding from the Award in Pain allow you to do?
Long after patients have healed from the primary phase of acute pain following an injury, some patients experience relapse and recurrent episodes of severe pain. The recurrent nature of chronic pain is poorly understood and has been under-investigated.
The funding from the Award in Pain is a tremendous opportunity for us because it will allow us to move forward investigating what prevents pain from re-emerging after remission. We have developed a new mouse model to study the remission and relapse of pain. We hypothesize that during the remission of pain, anti-inflammatory molecules are produced to block the inflammation and also activate the endogenous opioid system (our body naturally produces opioids such as endorphins). Understanding why chronic pain recurs will help lead to the development of therapeutics to alleviate chronic pain.
How did you enter this career path? Was there anyone or anything that particularly inspired you?
I have always been passionate about life sciences. As a kid, I dreamt of becoming a zoologist discovering new species. In college, I became more interested in the biomedical field and the opportunity to help people suffering from incurable diseases. I studied mostly genetics and molecular biology. My interest in neuroscience emerges from the basic question of how changes at the molecular or cellular level translate into long-term alterations in behavior. Driven by this question, I enthusiastically joined a lab studying chronic pain with the aim to understand what changes at the molecular level lead to the transition from normal perception to chronic pain hypersensitivity.
What is your favorite science-related book?
The Third Chimpanzee: The Evolution and Future of the Human Animal by Jared Diamond—not specifically related to pain, but it inspired my interest in the biological basis of human behavior and associated diseases.
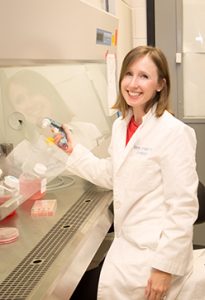
Photo: Cathleen Rueckeis
Sarah Linnstaedt, University of North Carolina at Chapel Hill
Assistant Professor, Anesthesiology
B.S., Virginia Tech
Ph.D., Georgetown University
In conjunction with Open Philanthropy
Almost all individuals will experience at least one traumatic injury in their lifetime. While the majority of these individuals recover, a substantial subset develop chronic post-traumatic pain (CPTP). We are interested in better understanding how to predict which individuals will recover versus develop CPTP following trauma, and how to prevent CPTP in those at high risk. To address this goal, we use translational research approaches to discover genetic and molecular vulnerability factors that predict CPTP and to identify promising targets for therapeutic preventative interventions.
What will funding from the Award in Pain allow you to do?
I am extremely excited to have been selected as a recipient of the 2020 Award in Pain because the awarded funds will provide us the opportunity to perform studies that assess whether a stress system protein, FKBP51, is a promising target for the prevention of CPTP following traumatic stress exposure. Preliminary data from our group and others indicates that inhibition of FKBP51 reduces CPTP and other types of pain, but important additional studies on the timing of inhibition, mechanisms, and safety are needed to further advance this work. Award in Pain funding will be an important conduit in progressing these studies to the next stage of development.
How did you enter this career path? Was there anyone or anything that particularly inspired you?
I was very fortunate to join the University of North Carolina at Chapel Hill Anesthesiology Research group in 2012, after transitioning from a postdoctoral fellowship in which my research focused on other types of human health. Mentoring from and collaboration with Samuel McLean at UNC-CH enabled me to learn the necessary knowledge and skills relevant to the pain field and to study molecular and genetic predictors of CPTP in longitudinal human cohort studies. This important educational foundation and human cohort work was the catalyst for the current laboratory-based studies we are now pursuing.
What is your favorite science-related book?
I would have to say my favorite science-related book is The Hot Zone: The Terrifying True Story of the Origins of the Ebola Virus by Richard Preston, because it inspired my initial interest in research. I read this book when I was in my first year of high school, and after finishing the book needed to know all the how’s, why’s, and what’s of disease pathogenesis. Currently, my lab team is reading The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk, and we discuss it during a monthly book club meeting. We enjoy reading this book because it provides clinical vignettes describing how trauma can affect an individual and lead to the development of adverse neuropsychiatric outcomes that are related to CPTP.

Photo: Nicholas Nguyen
Andrew J. Shepherd, The University of Texas MD Anderson Cancer Center
Assistant Professor, Department of Symptom Research
B.S., The University of Manchester Institute of Science and Technology, United Kingdom
Ph.D., The University of Manchester, United Kingdom
My work focuses on how injury, inflammation, and cancer interact with the nervous system to cause pain. We are particularly interested in how chronic illnesses disrupt the immune system, thereby increasing pain risk. Macrophages, a type of immune cell, are important contributors to pain. Macrophages infiltrate damaged tissue to clear debris and infection. Ordinarily, this process eventually resolves, promoting healing. We hypothesize that chronic pain often stems from macrophages failing to make this transition from a “damage response” to a “pro-repair” state. In such cases, macrophages continually sustain inflammation, causing nearby nerves to remain hyper-excitable and drive chronic pain. Our knowledge of these mechanisms is surprisingly limited, a problem that is set to become more widespread as chronic illnesses and cancer survivorship improve. We hope that improving our understanding of these “neuro-immune” interactions will identify novel therapeutic targets and facilitate the development of safe and effective analgesics.
What will funding from the Award in Pain allow you to do?
We can accelerate progress in two cancer-related lines of inquiry where we have already gathered some interesting findings. Pain associated with the metastasis of prostate cancer to the bones is often treated using opioids and bisphosphonates (to preserve bone density), or broad-spectrum immunosuppression, each of which have their limitations. With this award, we will gain insight into specific inflammatory processes caused by metastases and their contribution to pain. We will build a list of inflammatory molecules that are responsible for causing bone pain when prostate cancer metastasizes. We will also gain insight into how these products of inflammation increase neuronal excitability, a major contributor to the debilitating pain associated with bone metastasis.
Our second project focuses on the pain caused by cancer chemotherapy, using a mouse model of colon cancer. The chemotherapy drug oxaliplatin is effective at increasing overall survival in colorectal cancer, though a subset of patients go on to develop chronic pain due to nerve injury. What causes some patients to recover and others to develop chronic pain is unknown. Using this award, we will be able to search for hallmarks of inflammation associated with cancer that predispose the patient to the development of pain following chemotherapy, potentially identifying risk factors and new therapeutic interventions.
How did you enter this career path? Was there anyone or anything that particularly inspired you?
I consider myself fortunate to have been able to train under numerous role models throughout my scientific career. If I had to pick just one, it would be Carys Bannnister, who, by the time I met her, was a retired neurosurgeon. She continued to visit the lab where I was a graduate student several times a week to conduct experiments and act as an ad hoc mentor. She was incredibly knowledgeable, enthusiastic, and compassionate, with a keen eye for detail and a relentless focus on the clinical relevance of our research. I aspire to be that kind of mentor to the trainees in my lab.
What is your favorite science-related book?
The Selfish Gene by Richard Dawkins deserves an honorable mention for the elegant, entertaining way it explains the diversity of life on earth. However, when I give neuroscience lectures, I always find an opportunity to work in a reference to The Man Who Mistook His Wife for a Hat, by the famed neurologist Oliver Sacks. He weaves together stories from his time in the clinic about the effects of neurological injury. It focuses on the often profound changes to his patients’ perceptions and behaviors, but he also takes time to address the effects on the loved ones who care for them. It’s an amazing blend of fascinating, poignant, and occasionally hilarious observations.